Measure. Act. Impact.
Turnkey Collaborative Care for Providers
Increase access to behavioral health support and drive revenue. Everything you need to make the Collaborative Care Model (CoCM) work, in one place.
Addressing Behavioral Health in Primary Care
Up to 70% of primary care visits are driven by mental health concerns. Primary care providers (PCPs) are burdened by the extra time this requires, the inability to get additional mental health support to patients that need it, and the complexities of treating patients with co-morbidities.
Fortunately, you don’t have to be in this alone. The Collaborative Care Model (CoCM) offers a patient-centric, evidence-based model of integrated care designed to identify and treat patients with behavioral health conditions using a multi-disciplinary care team.
PROVEN BENEFITS
The leading model for Integrated Behavioral Health
CoCM is a care model proven to benefit patients, providers, and practices
-

Increase access to mental health care
It’s no secret that accessing mental health treatment can be weeks - or even months! - long. With CoCM, you can offer quick access to support when patients present with mental health concerns.
-

Improve outcomes for patients
The burden of a mental health condition can exacerbate physical symptoms and conditions. A patient-centric approach, CoCM offers a whole-person perspective proven to help patients feel better, faster.
-

Generate additional revenue
Collaborative care has a 6:1 ROI for the healthcare system. So, CMS and all major insurance companies have authorized CoCM codes to better compensate you for the time spent treating mental health concerns.
-

Monitor treatment effectiveness
Mirah's platform enables care teams to regularly measure symptoms and outcomes, allowing you to monitor the effectiveness of treatment and make adjustments as needed.
-

Increase provider satisfaction
Built-in support for patients with behavioral health needs means PCPs save critical time. PCPs also enjoy additional benefits like hared learning and the ability to treat to the top of their licensure.
-

Reduce overall burden on providers
A multi-disciplinary care team relieves administrative burden on PCPs around documentation, follow-ups, and supporting other essential elements of care, such as concerns around social determinants of health.
Measure both clinical outcomes and financial sustainability metrics.
Automate the digital sending, scoring, graphing, and analysis of over 500 clinically validated measures in Mirah’s library to assess a wide range of diagnoses (anxiety, depression, PTSD, etc.).
Aggregate outcomes data at the individual, unit, and organization level.
Set and track billing and reimbursable minute targets to optimize financial performance.
Monitor key implementation metrics such as case loads per care manager and enrollments by PCP.
Leverage Mirah’s billing insights report to track and optimize financial performance.
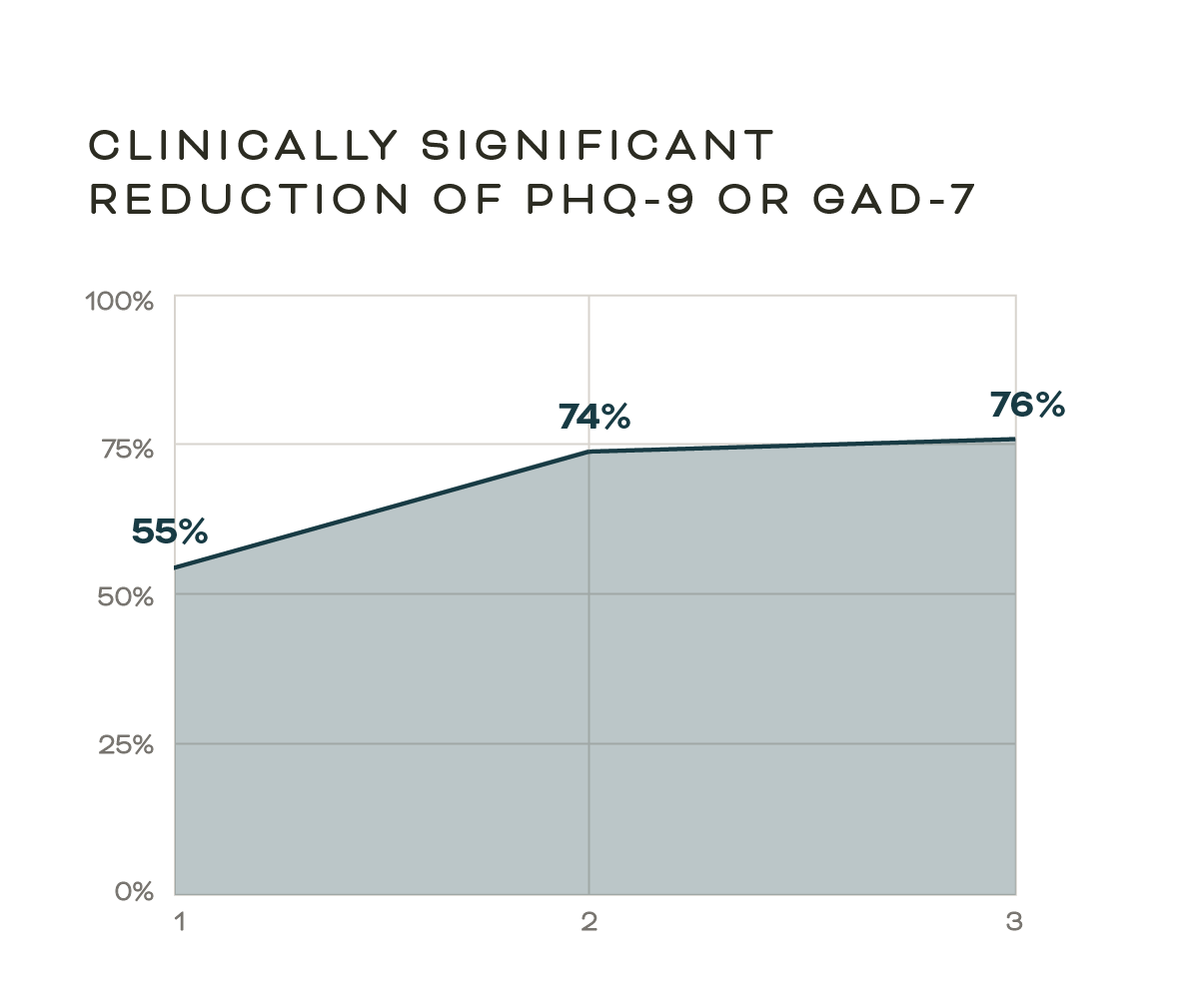
Months in Care
Act by guiding care managers to take the right actions at the right time.
Allow supervisors real-time insights into Care Manager performance.
Identify and prioritize patients needing attention and prompt appropriate actions
Know which patients are close to billing thresholds to ensure financial sustainability
Generate automated billing reports with the exact codes for each patient.
Impact patient outcomes and drive revenue for your practice.
Improve and report on patient outcomes by personalizing treatment with data-driven insights.
Enhance care manager efficiency and increase caseloads, increasing the number of patients with access to care
Scale programs and boost revenue with automation and standardized workflows.
Maximize billable minutes through automated time tracking for care activities.